Medical myths are some of the hardest misconceptions to break, but with consistent and clear communication of the facts, and sharing the most accurate information with our peers and social networks, we can help dispel stubborn rumors and separate fact from fiction. Case in point: concerns and fears about the flu vaccine contribute to less than optimal vaccination rates across adult populations.
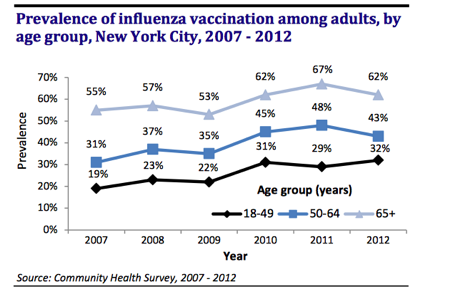
The influenza virus can cause significant illness, including hospitalization and death, particularly in high-risk groups such as younger and older persons, pregnant women, and those with certain chronic medical conditions. Flu vaccination is the most effective way to prevent transmission of the influenza virus, yet flu vaccination rates continue to hover around 40% among adults over the age of 18—well below the national target of 80% vaccination. According to the Centers for Disease Control and Prevention, flu vaccination coverage peaked at 43.6 % for adults 18 years and older in the 2014-15 influenza season. In New York City, adult vaccination rates fell well below national targets. According to the NYC Community Health Survey, which trends data from 2007-2012, those rates are rising, but they continue to fall below the goals established by the US Department of Health and Human Services.
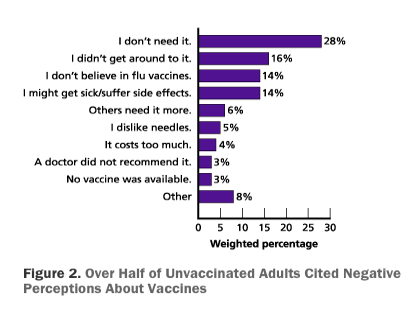
In a survey of unvaccinated adults in the 2009-10 flu season, researchers found that that over half of unvaccinated participants did not receive the vaccine not because they were unable to but because of its perceived lack of value. Among the reasons cited were many negative perceptions about vaccines (see the figure below).
Common misconceptions about the flu include:
- The flu vaccine causes the flu.
False. The flu vaccine is made either from inactivated viruses that cannot cause infection, or with no viruses at all in the case of the recombinant flu vaccine. The nasal spray vaccine contains attenuated (i.e. weakened) viruses that are cold-adapted, which means they are designed to cause only mild infection at cooler temperatures in the nasal passages but cannot infect the lungs or other parts of the body where warmer temperatures exist.
The most common side effects of the flu vaccine are mild. They include redness, soreness, tenderness or swelling at the shot site. Some people may experience low-grade fever, headache and muscle aches, but they are short in duration. The nasal spray vaccine is also well tolerated. It may cause mild symptoms such as runny nose, nasal congestion and cough.
It takes about one to two weeks to build up immunity from the flu shot. If a person experiences flu-like symptoms after vaccination, it is likely because of influenza exposure prior to the vaccine being given or during the two-week period when protection is not yet established. In some cases, a person may be exposed to a flu virus that is different from the viruses the vaccine is designed to protect against. Also, in people age 65 or older and those with weakened immune systems, the vaccine may not provide adequate immunity. For older adults, a high-dose vaccine is available, which may provide more effective protection throughout the flu season by creating a stronger immune response.
2. Healthy people don’t need to get vaccinated.
False. The Advisory Committee on Immunization Practices (ACIP) recommends an annual flu vaccine in people 6 months of age and older. Vaccination is recommended annually because immunity from the vaccine declines over time and the virus may mutate (i.e. change) from season to season. Vaccination is the most effective way to prevent transmission of the flu virus.
In addition to vaccination, you can protect yourself during the flu season by washing your hands frequently, and a health care provider may recommend the use of anti-viral medications, if you were exposed to an infected person prior to receiving the vaccine.
Some people may be infected with the flu virus and not show any symptoms. During this time, you are still contagious and may infect others.
Health care workers are routinely advised to get vaccination to reduce the risk of exposure to their patients. Also, vaccination helps prevent disease in family members who may be at higher risk of adverse outcomes. In particular, flu can cause serious illness in young children, pregnant women, older adults and people with certain medical conditions, such as asthma, diabetes or heart disease. However, the flu infection can carry a risk of serious complications even among healthy people.
3. The flu vaccine doesn’t have any real benefits.
False. While the flu vaccine is needed to prevent infection, it may reduce the risk of serious complications, especially in those who are more vulnerable to disease. In otherwise healthy people, the flu vaccine may make your illness milder, if you do get infected. Flu vaccination is an important preventive tool and saves lives and reduces morbidity (i.e. serious health outcomes). It is safer to be vaccinated than to risk infection and possible spread to others.
4. It’s too late now to get vaccinated.
False. While you should get vaccinated as early as possible in flu season, the flu vaccine will provide a benefit as long as flu viruses are circulating. ACIP recommends vaccination as soon as the vaccine becomes available, typically in October. While flu activity may peak in the winter months, between December and February, outbreaks can last as late as May. So, yes, you still have time to get protected and prevent infection.
Learn more
President Gresham Rolls Up for a Flu Shot at Brooklyn’s Maimonides Hospital
Misconceptions about seasonal flu and flu vaccines
No more excuses: you need a flu vaccine
Seasonal flu vaccination: why don’t more Americans get it?
Common misconceptions about the flu include: